Atherosclerosis is a chronic inflammatory disease of the arteries characterized by the accumulation of lipids, cholesterol, calcium, and cellular debris within the inner walls of arteries. This process leads to the formation of plaques, which can restrict blood flow and cause various cardiovascular problems. Here's a detailed look at the biology of atherosclerosis:
1. Initiation of Atherosclerosis
- Endothelial Dysfunction: The process begins with damage to the endothelium, the thin layer of cells lining the blood vessels. This damage can be caused by factors such as high blood pressure, smoking, diabetes, high cholesterol, and inflammation.
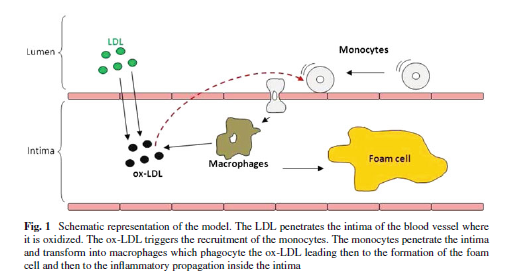
- Increased Permeability: Once the endothelium is damaged, it becomes more permeable to lipoproteins, particularly low-density lipoprotein (LDL) cholesterol. LDL particles penetrate the endothelial layer and accumulate in the subendothelial space.
2. Lipid Accumulation and Oxidation
- LDL Oxidation: Inside the arterial wall, LDL particles undergo oxidation, a process that makes them more atherogenic. Oxidized LDL (oxLDL) is highly inflammatory and contributes to the recruitment of immune cells.
- Foam Cell Formation: Macrophages, a type of immune cell, are attracted to the site of oxLDL accumulation. They engulf the oxLDL particles, transforming into foam cells. These foam cells are a hallmark of early atherosclerotic lesions, known as fatty streaks.
3. Inflammatory Response
- Cytokine Release: The presence of oxLDL and foam cells triggers the release of pro-inflammatory cytokines, which further amplifies the immune response. This leads to the recruitment of additional immune cells, including more macrophages and T-cells, to the site.
- Chronic Inflammation: This ongoing inflammatory process drives the progression of the atherosclerotic plaque, leading to the formation of more foam cells and the recruitment of smooth muscle cells from the arterial media layer.
4. Plaque Formation
- Fibrous Cap Formation: Smooth muscle cells migrate to the intima (the inner layer of the artery) and proliferate, synthesizing extracellular matrix components like collagen. This forms a fibrous cap over the lipid core, which stabilizes the plaque.
- Calcification: As the plaque matures, calcium deposits can accumulate, further hardening the arteries and contributing to plaque rigidity.
5. Plaque Progression and Complications
- Plaque Growth: Over time, the plaque grows, narrowing the arterial lumen and restricting blood flow. This can lead to ischemic conditions, such as angina (chest pain).
- Plaque Rupture: In some cases, the fibrous cap may rupture, exposing the underlying lipid core to the bloodstream. This can trigger the formation of a thrombus (blood clot) at the site, which can completely occlude the artery, leading to a heart attack or stroke.
6. Clinical Consequences
- Coronary Artery Disease: Atherosclerosis in the coronary arteries can lead to coronary artery disease (CAD), the leading cause of heart attacks.
- Cerebrovascular Disease: When atherosclerosis affects the carotid arteries or other vessels supplying the brain, it can lead to stroke.
- Peripheral Arterial Disease: Atherosclerosis in arteries supplying the limbs can lead to peripheral arterial disease (PAD), causing pain, ulcers, and even limb loss.
7. Risk Factors and Prevention
- Modifiable Risk Factors: Lifestyle factors such as smoking, poor diet, lack of exercise, and obesity significantly increase the risk of atherosclerosis. Managing these risk factors can reduce the likelihood of plaque formation.
- Non-Modifiable Risk Factors: Age, gender, and genetic predisposition also play a role. Men are generally at higher risk, though the risk for women increases after menopause.
- Medications and Treatment: Statins and other lipid-lowering drugs, along with anti-inflammatory agents, can slow the progression of atherosclerosis and stabilize plaques.
8. Advanced Therapies and Research
- Gene Therapy: Research is ongoing into gene therapy approaches to modify lipid metabolism or inflammatory responses to prevent or reverse plaque formation.
- Biomarkers: Identifying biomarkers for early detection and monitoring the progression of atherosclerosis is a key area of research.
In summary, atherosclerosis is a complex and multifactorial disease involving lipid accumulation, inflammation, and immune responses, leading to the formation of plaques that can cause significant cardiovascular diseases. Understanding these biological processes is crucial for developing effective prevention and treatment strategies.